Disclaimer: this post does not address the merits of the treatments proposed by the IHU team nor their risks, and even less the fact that Prof. Raoult would be a genius, a madman or a top scientist who got lost along the way.
It all started with a video, posted on February 25th, 2020, then entitled “Covid-19: endgame”, and put by IHU Méditerranée-Infection on Youtube. In that less than 2 mn video clip, extracted from the end of a seminar, Didier Raoult states that COVID-19 is “probably the easiest respiratory infection to treat” and that chloroquine (CQ) is effective and already “recommended for all clinically positive cases” in China. It wasn’t the first time this infectious disease star recommended CQ and its cousin molecule, Hydroxychloroquine (HCQ) to fight viral infections. Indeed, as early as 2007, he presented these drugs as “an interesting weapon to face present and future infectious diseases worldwide” in the International Journal of Antimicrobial Agents. (IJAA). Framed as a recycling of these antimalarial drugs, the article constituted a literature review, mainly of in vitro studies, and was part of the scientific and medical strategy of the IHU, the repositioning of old molecules, free of rights, towards new uses. And this possibility of reuse was taken up in a letter sent on February 11th, 2020 to the same journal (IJAA), accepted the same day and published on Februray 15th.
The series of IJAA publications continued. The day after the Youtube video, a new article was submitted, specifically dedicated to the use of CQ as a treatment for the COVID-19 epidemic. Accepted the next day, February 27th and published a week later, it repeated the efficacy claims observed by the Chinese and as a result of clinical recommendation. This assertion is based in particular on one of the strangest references I have ever encountered. Indeed, it is a letter of exactly ten lines published in BioSciences Trend, which body is copied below :
The coronavirus disease 2019 (COVID-19) virus is spreading rapidly, and scientists are endeavoring to discover drugs for its efficacious treatment in China. Chloroquine phosphate, an old drug for treatment of malaria, is shown to have apparent efficacy and acceptable safety against COVID-19 associated pneumonia in multicenter clinical trials conducted in China. The drug is recommended to be included in the next version of the Guidelines for the Prevention, Diagnosis, and Treatment of Pneumonia Caused by COVID-19 issued by the National Health Commission of the People’s Republic of China for treatment of COVID-19 infection in larger populations in the future.
Defined as an “abstract” on the journal site, but without any other body of text, this “article” doesn’t seem to be fully supported by the 7 references listed. It relies mainly an in vitro study from early February, already widely cited, which indicates that CQ could be effective. In fact, It wasn’t until February 29 that the results of a CQ clinical study were submitted to a Chinese journal, before being published on March 6. But let’s go back to the IHU timeline.
Ten days later, a second video was put on Youtube, presenting the results of an observational study made in Marseille and showing the effects of HCQ alone and in combination with an antibiotic, azithromycine (AZ). So there was a slight shift: going from CQ to HCQ and adding an antibiotic. The main result is only the absence of virus in nose and throat, so it is not clinical results but Didier Raoult drew from results to tell his audience their consequences for the clinical institution he manages:
“The fact that you no longer have the virus changes the prognosis. Actually, that’s what infectious diseases are all about. If you don’t have the germ anymore, you’re saved… You have a right to be tested here, and if you’re tested, you have a right to be treated here. That is what we will do.“
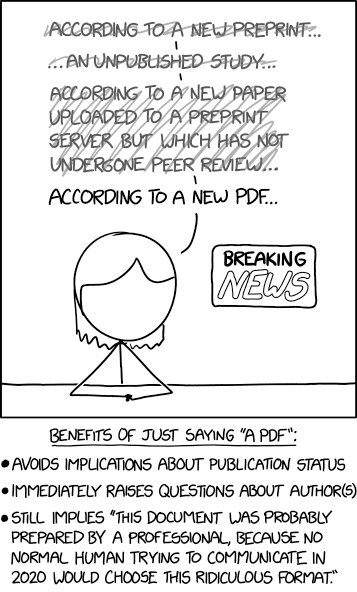
So basically, for him, results were so good that you HAD to treat people when they are tested positive. No more trials or research needed, the time for clinical medicine had come, hoping other places would follow his lead. Slides were available on the same webpage but no link to an existing paper, though the same day, but not mentionned in the video, a preprint was submitted to MedrXiv Simultaneously, as it is often the case with biomedical preprints, it was submitted to a journal… the ever-welcoming IJAA, who accepted it, as usual, one day later and published it on March, 20th. Before we come to the extraordinary fate of this paper, let us go back to the title of this post and its interest at this point.
From preprints to preprints:
the life and dearth of the Ingelfinger rule
We can observe from the two examples above a pattern of scientific communication: the IHU first posts videos, then produces preprints and finally publishes articles in academic journals – here IJAA. This is very unusual, at least in contemporary times, but happened in various ways during centuries of scholarly communication. The idea that you had first to communicate with your peers through a journal before getting to “the public” is neither constant nor dominating in all disciplines. In our era, it was pushed at a key moment in the mid-1960s. Back then, a first wave of preprints was being supported by NIH and was gaining momentuml in some biomed communities through Information Exchange Groups (IEG) that would circulate by air mail printed copies of unpublished manuscripts1. Nature started a campaign against the “preprint galore” and a few European and US biology and biochemistry journals editors-in-chief met in Vienna in 1966 to get rid of them by stating that : “The journals listed below will not consider manuscripts for publication if preprints, of essentially identical content, are to be distributed, in substantial numbers, by an agency independent of the author or of the publisher of the journal. “2
That led to the termination of the IEG experiment by the NIH in 1967. Two years later, the New England Journal of Medicine (NEJM) editor-in-chief, Franz J. Ingelfinger, coined the rule of acceptance of a paper, based on his interpretation of “sole contribution”, de facto forbidding even “circulation-controlled journals” to print something ahead of the NEJM3. In the same sentence, he remarkably included “news media”: he therefore aimed not only at the exclusive circulation of the article within scientific communities, but also to the prohibition of dissemination of its content to journalists and other medical news enthusiasts. In the early 1970s, his work to promote this exclusivity had a double effect: this practice was given the name Ingelfinger Rule, and many high-profile journals adopted it explicitely. While at the beginning of the 21st century the Ingelfinger Rule was often interpreted as a means to fight against the duplication of papers, its aims were more about controlling the circulation of knowledge in order to protect the newsworthiness of “general medical journals”4 and to organize communication about medical academic papers in a specifc way, favorable to a limited number of journals.
Indeed, as Vincent Kiernan beautifully described in his 1997 article5, the Ingelfinger Rule had become prevalent in Anglo-American journals. It is in particular the efforts of the International Committe of Journal Medical Editors (ICMJE) that built it as a “publishing standard”, which effect was for these journals and their editors-in-chief to simultaneously operate a double control:
- control on the authors by requiring them not to reveal the content of their articles, and even less so share the figures and other synthetic representations of results.
- control on journalists by providing them with preprint copies of articles in advance, while imposing an embargo on them until actual publication by the journal.
As a result, the general press (free of charge) advertises the content of the journals – it is not an article by Dr. X & Y., but an article from the NEJM or The Lancet – and organizes the dissemination of “medical discoveries” by strengthening the influence of these journals both within academic communities and within press professionnals and the general public. To conclude his paper, Kiernan questions the durability of such practics in the Internet-era and points out the effect of ArXiv preprints, citing the efforts of the ICMJE to extend the Ingelfinger rule to e-prints, with the argument of the direct consequences of biaised or false medical knowledge for the public.
The biomedical field resisted 15 more years to preprints and the Ingelfinger Rule largely stood6, even if it was adapted to emergency contexts, such as the AIDS epidemic. But Kiernan’s forecast came into reality, notably with the creation of BiorXiv in 2013 and the subsequent success of preprints in biology and biomedicine, until preprints became quasi-articles. Consequently, the Ingelfinger rule was dropped by numerous journals and publishers, even if NEJM itself keeps a case by case policy.
Prof. Raoult and his videos, possibly including slides with the figures so dear to the NEJM, thus live in a post-Ingelfinger world, in which academics can directly ensure their communication, not only in terms of content, but also in terms of comments, criticism, reporting or response. Indeed, we will see that the primary communication is not the only one modified by the abandonment of this rule, but the complete organization of the journal’s centrality in the whole chain of scientific communication.
Chaos and creation around one paper
Let us go back to this first publication by Raoult’s team on the effects of HCQ on viral porting, published in the IJAA on March 20, 2020. At the time of writing this post, the article has received 1124 citations according to Google Scholar but also thousands of tweets, blog posts and other references in press articles according to PlumX, a company owned by Elsevier, itself the IJAA publisher. The early circulation of the article was not based on a press release of the IJAA, but on Raoult’s own video and that of his various networks. As Wired recounts, with the help of a lawyer, a retired doctor, a shared google doc and an interview to Fox News, an heterogeneous assemblage à la Bruno Latour, the study published in the IJAA won a quote in a Tweet from the President of the United States the day after its publication:
That Trump endorsement of course had enormous consequences on the HCQ market, the launching of clinical trials, self-medication HCQ practices and the scope of public discussion on the efficacy and dangers of such a treatment. We won’t directly treat these important questions here, but keep on following the exotic trajectory of the publication itself. Simultaneouly to the Trump tweet, a PubPeer thread was lauched on the famous post-publication comment platform, but contrary to the Voinnet affair7, most of the first commentators signed their critiques. Among other topics, the communication trajectory of the paper helped the critique: for example, Leonid Schneider noticed the discrepancies between the figures attached to the video and the ones drawn in the published paper.
Above and beyond Pubpeer, three reviews were quickly published, questionning many aspects of the IJAA paper. The first one is a twitter thread by a master student on March, 22nd ; the second one is a zenodo 18-pages paper by three British/Irish statisticians on March, 23rd ; the third one was a blog post by a very famous Dutch microbiologist and scientific misconduct specialist, Elizabeth Bik on March, 24th. So only four days after publication – still four times the actual reviewing IJAA delay – the paper is being trounced online. Among the many points, let us note that the publishing history was being questioned, some noticing the differences between the first “preprint” on IHU website and the final paper, others underlying the lack of changes, an hint for them on how tenuous the peer review process has been., the 24h delay being surprising to every commentator. The fact that one of the authors was also the editor-in-chief of IJAA was underlined, as well as the “vanishing” of 6 patients (among 26 treated by the combined drugs), which could completly change the statistical value of the results.
While Prof. Raoult was fighting for HCQ to be authorized for general physicians in France, the online discussion kept on going until the learned society, the International Society of Antimicrobial Chemotherapy (ISAC) behind the journal, made a troubling press relase on April 3rd:
“ISAC shares the concerns regarding the above article published recently in the International Journal of Antimicrobial Agents (IJAA). The ISAC Board believes the article does not meet the Society’s expected standard, especially relating to the lack of better explanations of the inclusion criteria and the triage of patients to ensure patient safety. Despite some suggestions online as to the reliability of the article’s peer review process, the process did adhere to the industry’s peer review rules. Given his role as Editor in Chief of this journal, Jean-Marc Rolain had no involvement in the peer review of the manuscript and has no access to information regarding its peer review. Full responsibility for the manuscript’s peer review process was delegated to an Associate Editor. Although ISAC recognises it is important to help the scientific community by publishing new data fast, this cannot be at the cost of reducing scientific scrutiny and best practices. Both Editors in Chief of our journals (IJAA and Journal of Global Antimicrobial Resistance) are in full agreement.”
So the paper has a lot of problems, but stuck by the peer review rules. This cryptic PR became even more troubling a week later as it was “replaced” by an ISAC and Elsevier press release. In fact, the journal is not owned by the learned society, but by the Publisher, only being an “official society journal”. This second PR is streamlined compared to the first one as the “not meeting standard” sentence has disappeard and an announcement of post-publication peer review audit. Through this example, we measure how much different is the situation from what was prevalent under the Ingelfinger Rule. But it is with another Raoult’s team paper that science communication came back to its 17th century roots.
From presidential visit to media frenzy:
the marginalization of journals in scholarly communication
After a follow-up study published at the end of March which made less headlines and as some HCQ trials on diverse patient groups were starting to being published, it is with another observationnal study that Prof. Raoult showed the world how he was really managing scholarly communication. On April 9th, the French president, Emmanuel Macron unexpectidely visits IHU Mediterrannée and meets with Prof. Raoult, who presents him the results of its ongoing study. There was no press, but members of the IHU had recorded the arrival of Macron and posted it, making it available to the whole French media.
Here we need to go back to the origins of scientific communication, even before journals were born, when the quality of witnesses – meaning mostly royalty kinship – were an important element of the credit given to the narrative of an experiment or an observation8. In our times, it became a two-way credit flux: Macron was showing his will to base public health on evidence-based, all the more given by a star scientist, while Raoult was legitimizing his position in the French public health landscape, where critics of his methods and results were numerous.
The next day, Raoult made public his first results, not in the form of a preprint or slides with an associated video, but as a simple tweet with the abstract and a summary table.
This tweet was of course massively picked up, commented on and aroused strong media interest, all the more so as the results reinforced those of the previous study by moving from a purely biological effect to a clinical effect: “The HCQ-AZ combination, when started immediately after diagnosis, is a safe and efficient treatment for COVID-19, with a mortality rate of 0.5%, in elderly patients. It avoids worsening and clears virus persistence and contagiosity in most cases. ” Four days later, Prof. Raoult was invited in Dr Oz show, a famous TV host in the US, harshly criticized for his often unproven medical advice.
At the day of the interview, there was no preprint and the paper was not even submitted to a journal. Yet, Prof. Raoult presents his results as facts. It was only on the 20th that the manuscript was sent to Travel Medicine and Infectious Disease,9, with 10 days for peer review and a publication on May, 5th. Tens of thousands of comments on Facebook and tweets have followed according to PlumX,10 though media as much endorsed the results as they reported the methodological limits os the study – mostly the absence of a control group.
This study is undoubtedly a borderline case in the marginalization of journals, with communication aimed primarily at peers being out of step with announcements to political leaders and media outlets. Nevertheless, the massive availability of preprints, abstracts or other materials on topics such as the effectiveness of masks or tests, the persistence of coronavirus on this or that surface, or cases of cure, has led to significant media coverage. From the point of view of the public authorities and the general public, it could have strengthened the authority of academic journals, again in a position to assert their necessity as a obligatory passage point for public dissemination. But this return to grace assumed that the journal peer review is an effective barrier against “bad science”, an hyptohesis which has been dismissed by thirty years of studies and literature.
Prestige journals in epidemic times:
an economy of reputation crumbling down?
Indeed, prestige journals are bad for methodology: they don’t follow their own standards on reporting clinical trials, and more generally disicplinary standards. Yet they remain prized places to publish, even during the pandemic where preprints are so trendy because of the urgency to share results and knowledge. And some HCQ papers have been quietly published in such journals, until one observationnal study seemed to close the dabate on this treatment efficacy and risks.
For this study, there was no advance communication, no preprint but a straight article published in The Lancet by 4 authors. Oh, yes, there is a little gem still there on Twitter : two days before online publication, the “first author” answered a tweet by Richard Horton, editor-in-chief of The Lancet:
The reaffirmation of their confidence in the journal peer review system, even in times of health emergency, is comforting. And their trust is shared by the highest health authorities. On May 22nd, the study was published and asserted on the basis of a gigantic aggregation of almost worldwide patient databases that HCQ is not only inefficient, but also a very dangerous for COVID-19 patients. This announcement came at a time when many ongoing trials are displaying HCQ treatment arms. As a result, the WHO decided the next day to evaluate the continuation of its Solidarity study and announced its position on May 25th:
“Having met on 23 May 2020, the Executive Group of the Solidarity Trial decided to implement a temporary pause of the hydroxychloroquine arm of the trial, because of concerns raised about the safety of the drug. This decision was taken as a precaution while the safety data were reviewed by the Data Safety and Monitoring Committee of the Solidarity Trial. “
Nevertheless, in a manner similar to Prof. Raoult’s article, statisticians then look at the content of the article, the data it provides, and begin to point out obvious errors. But for some it was more a police investigation than data re-analysis: how can there be only 4 authors (and no acknowledgements) for such a study? Why are the hospitals involved not mentioned? What is this mysterious enterprise – Surgisphere – unknown until recently, which provides this data? What is the career of its manager and co-author of the paper? Putting apart questions about the company, 6 days after publication, they end up writing an open letter to the authors and the journal, signed by 201 colleagues and endorsed by James Watson11. They mainly point out the necessity to open the data, even more considering the extraordinary results, and describe obvious errors, questionning the quality of the database and the way (including ethics) data was gathered.
The Lancet and the authors were very prompt in responding to these criticisms: in fact, on May 30 a correction was published, covering very minor aspects. : “the numbers of participants from Asia and Australia should have been 8101 (8·4%) and 63 (0·1%), respectively. One hospital self-designated as belonging to the Australasia continental designation should have been assigned to the Asian continental designation.” Of course, the conclusion was a classic in those corrections : “There have been no changes to the findings of the paper.” But critics keep on pushing on the problems, would they be HCQ supporters, Prof. Raoult himself stating “fake data” or “manipulated data” on Twitter or clinicians trying to find coherence between the papers’ data and their own. So, only 3 days after the correction, The Lancet puts an expression of concern on the paper:
“Although an independent audit of the provenance and validity of the data has been commissioned by the authors not affiliated with Surgisphere and is ongoing, with results expected very shortly, we are issuing an Expression of Concern to alert readers to the fact that serious scientific questions have been brought to our attention”.
The paper was still saveable, thanks to the independant impeding audit. Alas, another 2 days and the 3 authors who do not belong to Surgisphere threw in the towel by stating they haven’t seen the data, and demanded the retraction of the article. The Lancet officialized it, provoking expression of outrage, the questioning of the seriousness of the journal and… the reactivation of the suspended trials. Thus, in less than a week, the worldwide study published in what many consider to be “one of the best medical journals in the world” has been awarded the 3 labels commonly used in post-publication peer review – Correction, Expression of Concern, Retraction12 – nullifying the evidence claimed on May, 22nd. But the Surgisphere story goes beyond that article: another paper, published by NEJM on the “same kind of data” was retracted on the same day. Moreover, there are at last two regions – South America and Africa – which have and will suffer from public health policies being developed on preprints and data published by Surgisphere. While #LancetGate was trending on twitter, in-depth inquiries were being made on Surgisphere and the 4th author of study who, ironically, coauthored a paper entitled : “Combating Fraud in Medical Research’ in 2013 !
Science at its best:
boring, negative results
To conclude this story on scholarly communication, we have to add that most HCQ articles have not been given the same media treatment and have not been communicated in fancy ways by authors: a preprint on BiorXiv or MedrXiv, then an article with often no spectacular results and limitations because of the number of patients, their previous health conditions, incomparability between groups, etc. One day before the retractions, the same NEJM published the first randomized-control trial on post-exposition use of HCQ, so close to the “Raoult treatment” – AZ not being included. Here is part of the abstract published:
“Side effects were more common with hydroxychloroquine than with placebo (40.1% vs. 16.8%), but no serious adverse reactions were reported.After high-risk or moderate-risk exposure to Covid-19, hydroxychloroquine did not prevent illness compatible with Covid-19 or confirmed infection when used as postexposure prophylaxis within 4 days after exposure.”
What do we get from this abstract? That the article is a typical example of those “negative results” that fail to be published, leading to significant biases in the evaluation of treatments in clinical trials through a “publication bias”13. And yet, not because of its own interest, originiality, breakthrough knowledge, but because of its relevance to public health in an epidemic situation, this trial has been published by the other “world’s best medical journal”.
While predictions of “really bad science to come” have sounded true for most commenters and supported by a high number of retractions, the COVID-19 academic publication landscape has also shown a massive uptake on preprints, public education on scientific controversies, conflict of interest and statistical analysis and furthermore… yes, publication of null results in prestige journals. Whether you think this is a total mess and you prefered the Ingelfinger rule depends on the way you conceive academic research and scholarly communication. Back then, preprints were non-existent in biology and social networks had to be invented, but The Lancet published the Wakefield paper on the link between MMR vaccine and autism. Was it a better time?
Cite this blog post
Didier Torny (2020, June 8). Living in a post-Ingelfinger world or… The HCQ-COVID-19 publication show. The political economy of academic publications. Retrieved April 19, 2024, from https://doi.org/10.58079/sy3a
- See Cobb, Matthew., 2017. “The prehistory of biology preprints: A forgotten experiment from the 1960s.” PLoS biology 15.11 [↩]
- Thorpe, W. V. (1967). International Statement on I nformation Exchange Groups. Science, 155(3767), 1195-1196. [↩]
- Ingelfinger, Franz. “Definition of” sole contribution”.” N Engl J Med 281 (1969): 676-677. [↩]
- Ingelfinger, F. J. (1977). The general medical journal: for readers or repositories?. New England Journal of Medicine, 296(22), 1258-1264. [↩]
- Kiernan, V. (1997). Ingelfinger, embargoes, and other controls on the dissemination of science news. Science Communication, 18(4), 297-319. [↩]
- See as an example this defense of the rule by Nature in 2010, five years after having written they were ok with preprint servers [↩]
- see Torny, Didier. “Pubpeer: vigilante science, journal club or alarm raiser? The controversies over anonymity in post-publication peer review.” 2018 and Guaspare, Catherine, and Emmanuel Didier. “The Voinnet Affair: Testing the Norms of Scientific Image Management.” Gaming the Metrics: Misconduct and Manipulation in Academic Research (2020): 157. [↩]
- See the classic book Shapin, S., & Schaffer, S. (1985). Leviathan and the air-pump: Hobbes, Boyle, and the experimental life (Vol. 109). Princeton University Press [↩]
- A journal in which one of the authors is an associate editor have underlined Raoult’s critics [↩]
- The story is quite different within the academic world with “only” 21 citations until now, far much less than the March study. In fact, many observationnal studies and trials were competing with this study [↩]
- EDIT June 9th: James Watson made a fantastic interview on an australian radio where he gets into detail about how he started and run this 5-days inquiry, hear it there [↩]
- On the standization of journal policies, see Pontille, D., & Torny, D. (2017). Beyond Fact Checking: Reconsidering the Status of Truth of Published Articles. [↩]
- There is a huge literature on this topic in the last 30 years, see as an example this The Lancet article, Easterbrook, P. J., Gopalan, R., Berlin, J. A., & Matthews, D. R. (1991). Publication bias in clinical research. The Lancet, 337(8746), 867-872. [↩]

